Tilted Implants in the Partially Edentulous Maxilla
The posterior maxilla can be a challenging area for implant placement due to the pneumatization of the maxillary sinus and the low density of remaining bone.1 Immediate loading in the posterior maxilla has shown a higher failure rate compared to implant loading in areas of better-quality bone.1 Sinus augmentation or overlay bone grafting may not provide the primary stability required for immediate function.2 Moreover, contraindications to sinus lift procedures — such as chronic sinusitis, tobacco use, pathologic lesions, odontogenic infections, anatomical abnormalities of the sinus and associated structures, and large prominent septa — pose challenging scenarios often associated with unpredictable outcomes.2,3,4,5
Use of short implants is a promising alternative, but caveats associated with biomechanics should be kept in mind. These issues include reduced bone-to-implant contact, especially in softer bone quality, and reduced force distribution, with more force concentration at the crest of the implant that can lead to greater resorption and greater risk of thread exposure.3,6,7,8,9
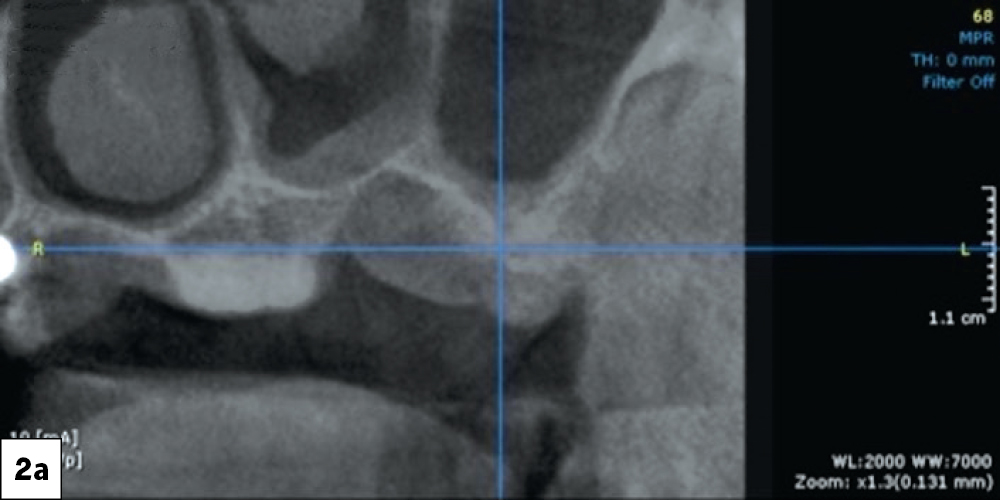
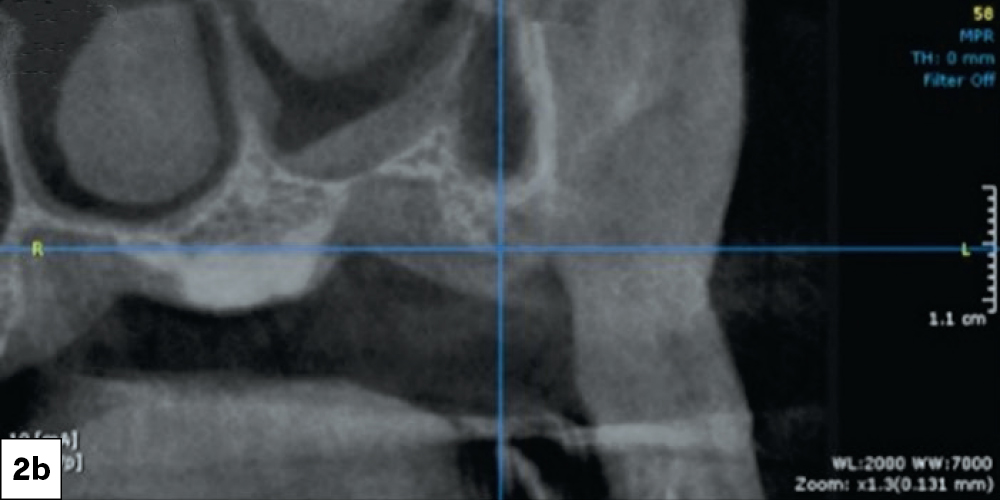
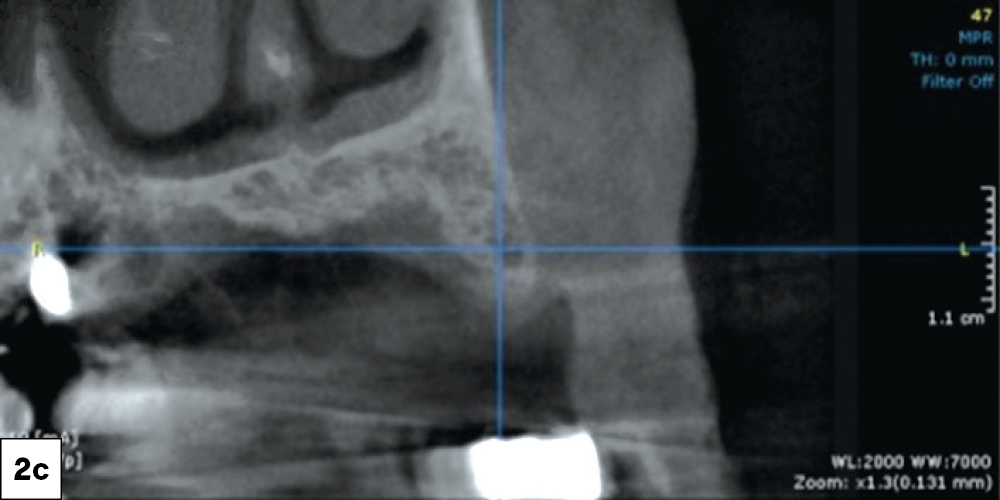
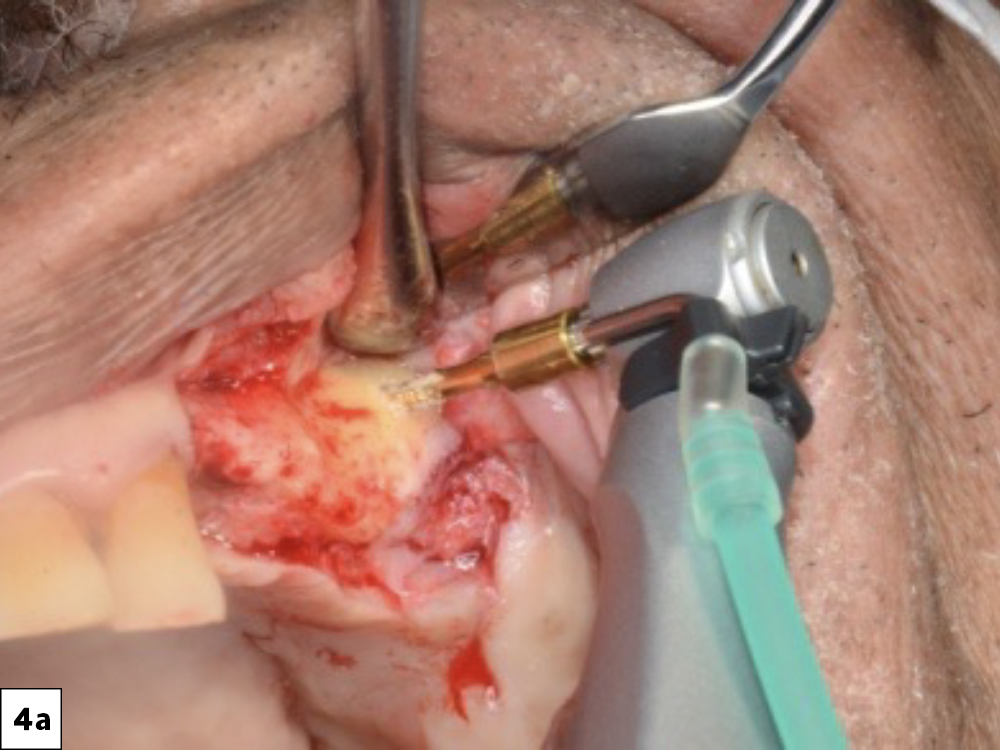
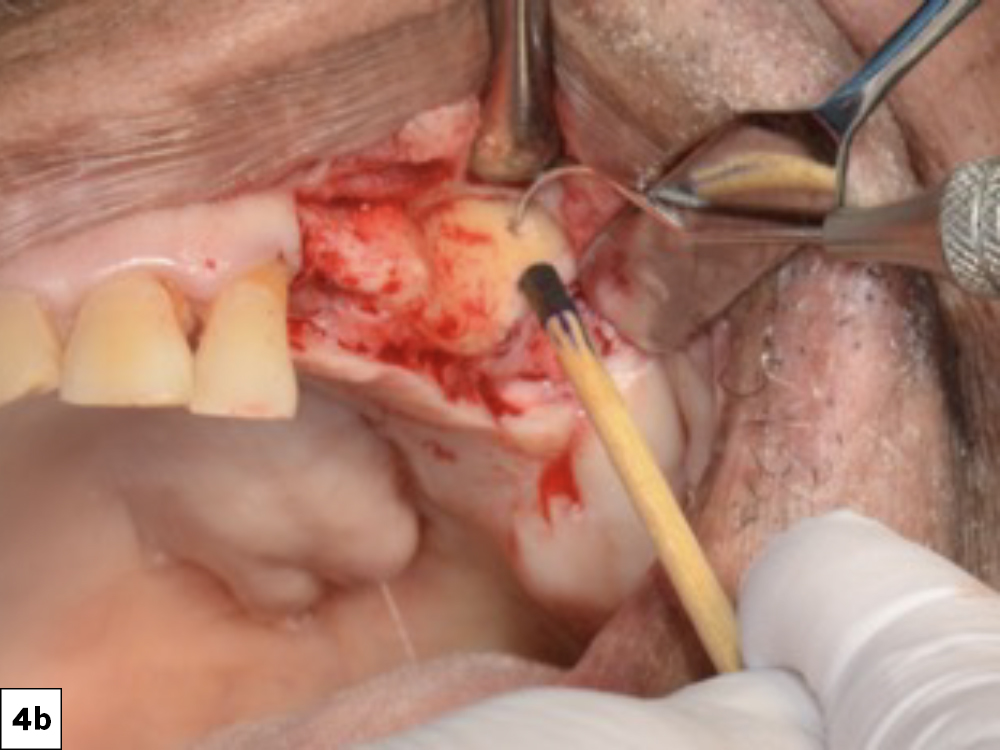
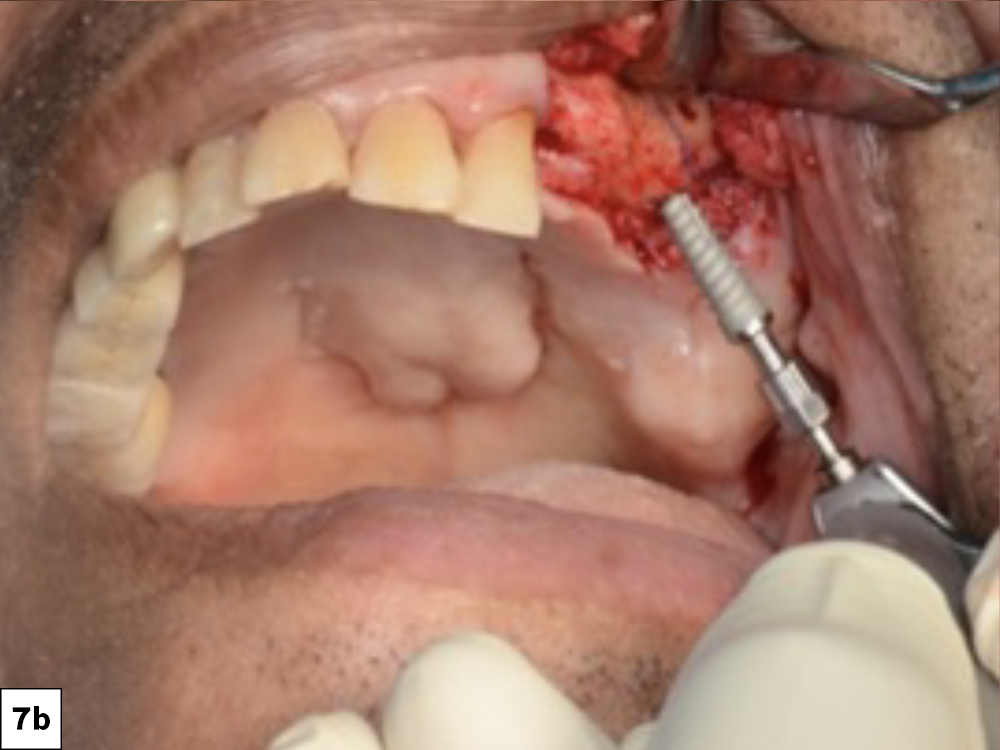
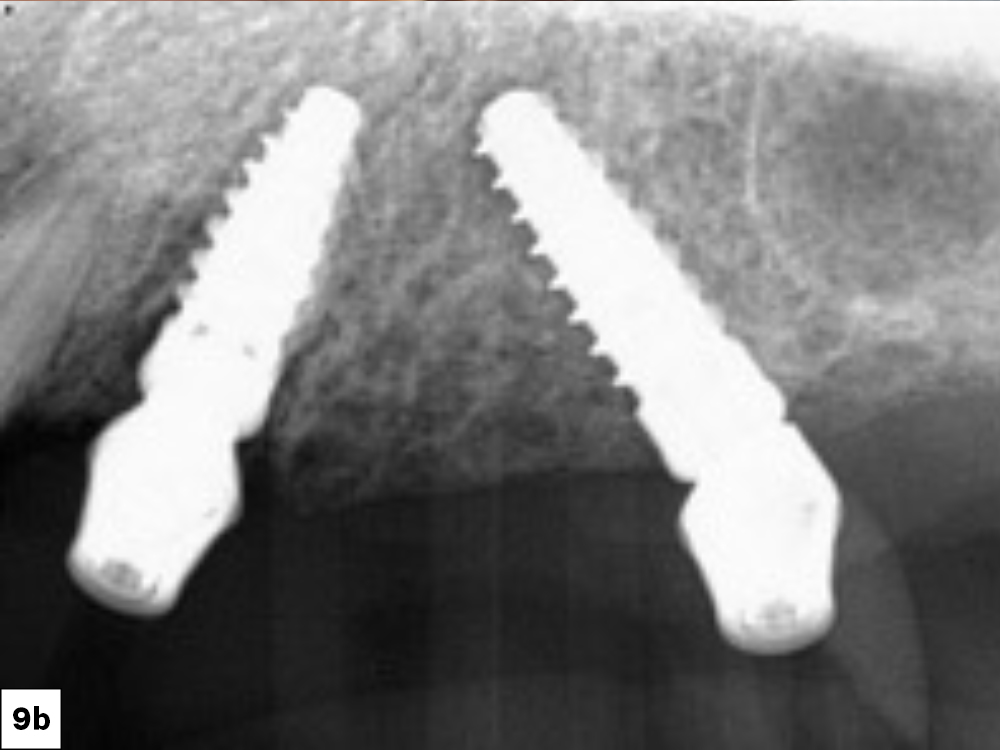
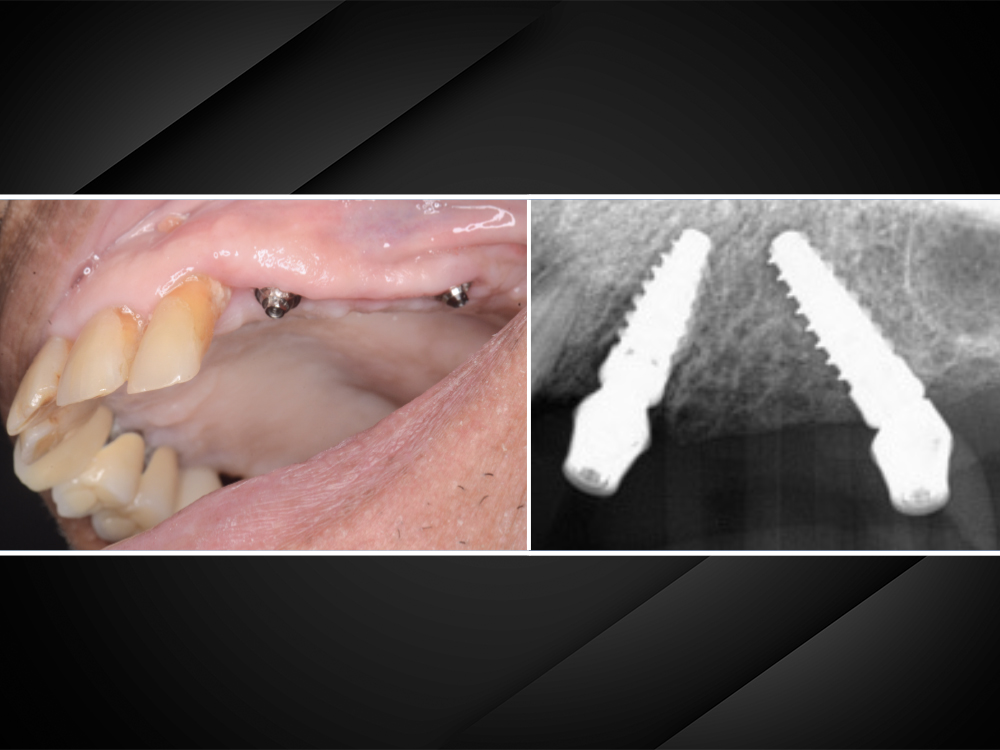
One alternative option enables treatment in a predictable and expeditious manner in the partially edentulous maxilla with reduced bone height. It involves using a combination of an axial implant in the anterior region and a tilted implant in the posterior region to support an implant-supported bridge. The placement of the posterior-tilted implant in partially edentulous situations should be in close proximity and parallel to the anterior wall of the maxillary sinus. The implant should be placed at an angle of 30 to 45 degrees, similar to completely edentulous scenarios of immediate loading.
Tilted implants have rendered predictable outcomes in completely edentulous scenarios for nearly 15 years.10,11,12 The benefits of tilted implants have also been noted in partially edentulous situations.13,14 There are several benefits associated with the use of tilted implants. Placing the implant at an angle enables placement of a longer implant. This provides greater implant engagement in the bone and increased bone-to-implant contact, which enhances the primary anchorage of the implant and enables immediate loading in many situations. This implant alignment often reduces bending moments by eliminating the need for a posterior cantilever. This in turn helps to attain a prosthetically favorable implant position while maintaining inter-implant distance.
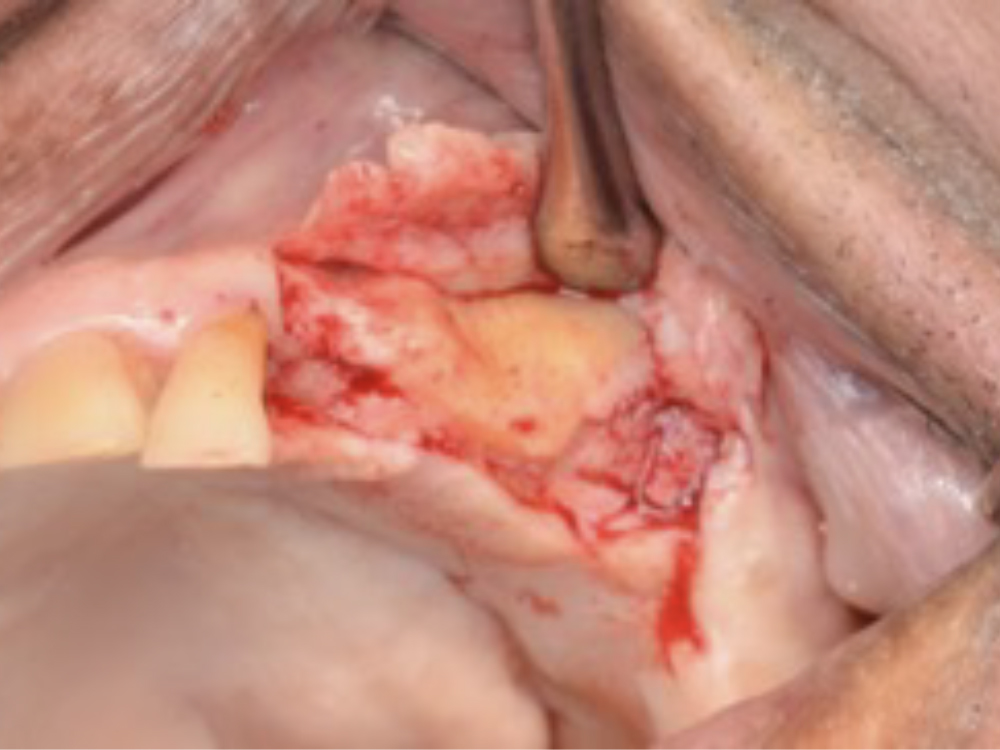
This case report demonstrates how utilizing angled implants that bypass the maxillary sinus for immediate loading can result in successful quadrant restorations. Some key elements to note when considering tilted implants and immediate loading include:
CASE REPORT
CONCLUSION
This case report demonstrates the use of a combination of axial and tilted implants to provide a graftless solution for a quadrant implant-supported restoration. The clinical indication for the use of tilted implants in the posterior maxilla is less than 5 mm of subantral residual bone height. Care should be taken that there is no severe alveolar ridge defect that would require major horizontal or vertical bone augmentation, and that a favorable interocclusal distance is present in such cases.1
Tilting the distal implant anterior to the maxillary sinus in this case led to achieving the emergence of the implant in the first molar region (#14) instead of the first premolar region (#13), where it would have emerged if axial implants were used in both sites. This achieved a longer span between the anterior and posterior implants, eliminating a cantilever design, while allowing for replacement of the optimal number of posterior teeth. The use of a tilted implant also rendered a stable biomechanical outcome by engaging a greater amount of bone than the alternative of using short implants. The engagement of bone enabled primary stability, which allowed me to immediately load the implants. The use of a tilted implant also eliminated the need for a sinus augmentation procedure, leading to a more efficient treatment with reduced surgical morbidity and expenses.
References
-
Anitua E. Immediate Loading of Short Implants in Posterior Maxillae: Case Series. Acta Stomatol Croat. 2017 Jun;51(2):157-62.
-
Avila-Ortiz G, Vegh D, Mukaddam K, Galindo-Moreno P, Pjetursson B, Payer M. Treatment alternatives for the rehabilitation of the posterior edentulous maxilla. Periodontol 2000. 2023 Jul 24.
-
Morand M, Irinakis T. The challenge of implant therapy in the posterior maxilla: providing a rationale for the use of short implants. J Oral Implantol. 2007;33(5):257–66.
-
Jensen SS, Terheyden H. Bone augmentation procedures in localized defects in the alveolar ridge: clinical results with different bone grafts and bone-substitute materials. Int J Oral Maxillofac Implants. 2009;24 Suppl:218–36.
-
Thoma DS, Cha JK, Jung UW. Treatment concepts for the posterior maxilla and mandible: short implants versus long implants in augmented bone. J Periodontal Implant Sci. 2017 Feb;47(1):2–12.
-
Telleman G, Raghoebar GM, Vissink A, den Hartog L, Huddleston Slater JJ, Meijer HJ. A systematic review of the prognosis of short (<10 mm) dental implants placed in the partially edentulous patient. J Clin Periodontol. 2011 Jul;38(7):667–76.
-
Thoma DS, Zeltner M, Hüsler J, Hämmerle CH, Jung RE. EAO Supplement Working Group 4 - EAO CC 2015 Short implants versus sinus lifting with longer implants to restore the posterior maxilla: a systematic review. Clin Oral Implants Res. 2015 Sep;26 Suppl 11:154–69.
-
Papaspyridakos P, De Souza A, Vazouras K, Gholami H, Pagni S, Weber HP. Survival rates of short dental implants (6 mm) compared with implants longer than 6 mm in posterior jaw areas: a meta-analysis. Clin Oral Implants Res. 2018 Oct;29 Suppl 16:8–20.
-
Mo JJ, Lai YR, Qian SJ, Shi JY, Lai HC, Tang GY. Long-term clinical outcomes of short implant (6mm) in relation to Implant Disease Risk Assessment (IDRA). Clin Oral Implants Res. 2022 Jul;33(7):713–22.
-
Krekmanov L, Kahn M, Rangert B, Lindström H. Tilting of posterior mandibular and maxillary implants for improved prosthesis support. Int J Oral Maxillofac Implants. 2000 May–Jun;15(3):405–14.
-
Maló P, Rangert B, Nobre M. “All-on-Four” immediate-function concept with Brånemark System implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5 Suppl 1:2–9.
-
Maló P, Nobre Md, Lopes A. Immediate loading of ‘All-on-4’ maxillary prostheses using trans-sinus tilted implants without sinus bone grafting: a retrospective study reporting the 3-year outcome. Eur J Oral Implantol. 2013 Autumn;6(3):273–83.
-
Apaza Alccayhuaman KA, Soto-Peñaloza D, Nakajima Y, Papageorgiou SN, Botticelli D, Lang NP. Biological and technical complications of tilted implants in comparison with straight implants supporting fixed dental prostheses. A systematic review and meta-analysis. Clin Oral Implants Res. 2018 Oct;29 Suppl 18:295–308.
-
Hämmerle CHF, Cordaro L, Alccayhuaman KAA, Botticelli D, Esposito M, Colomina LE, Gil A, Gulje FL, Ioannidis A, Meijer H, Papageorgiou S, Raghoebar G, Romeo E, Renouard F, Storelli S, Torsello F, Wachtel H. Biomechanical aspects: summary and consensus statements of group 4. The 5th EAO Consensus Conference 2018. Clin Oral Implants Res. 2018 Oct;29 Suppl 18:326–31.