Glidewell Dental Symposium 2017: Answers to Audience Questions

Doctors from around the country convened at the sold-out Glidewell Dental Symposium this past November in Dallas. A comprehensive range of topics critical to general dentistry were covered during the all-day event, and educators were available to answer attendee questions submitted through the symposium mobile app. Here, we present answers to some of the questions asked by the audience after hearing lectures covering digital dentistry, esthetic veneers, restorative material options, maximizing outcomes with provisionals, and more.
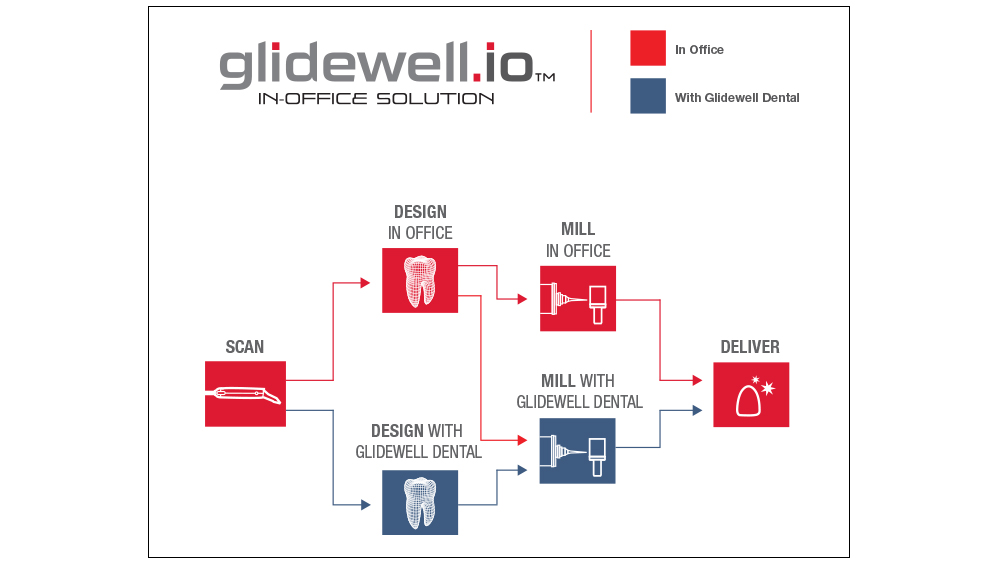
When utilizing the glidewell.io In-Office Solution, doctors have the flexibility to choose between creating and delivering restorations in-office or prescribing through Glidewell Dental, depending on the specific requirements of the case.
CHAD C. DUPLANTIS, DDS

In his presentation “Digital Dentistry: The New Office Paradigm,” Dr. Chad Duplantis discussed new restorative technologies and materials, and how dentists can utilize them to improve the services offered by their practices.
Have you noticed a return on investment with your in-office chairside milling system and, if so, how significant is it?
Dr. Chad Duplantis: Using the glidewell.io™ In-Office Solution (Glidewell Direct; Irvine, Calif.), the way I regard ROI, or return on investment, is twofold. First, I ask, “Is it a financial return on investment?” And the answer is, “Yes.” When we digitally send our scans to the dental laboratory, the restorations we receive are incredibly accurate and offered at a reduced fee. The digital workflow has allowed us to save on our lab bill by using an advanced yet affordable laboratory to fabricate the same quality restoration that a more expensive laboratory was fabricating for us. So, with that being considered, we’ve already saved money by purchasing the digital system for the cases that we send to the laboratory.
Second, I ask, “Have we saved money utilizing the chairside milling system?” And the answer again is, “Yes.” When we utilize intraoral scanning to create the digital file, which is used to design the restoration, we either digitally send the case to a laboratory or mill it in-office. When I take into consideration the number of restorations that our office does compared to what we did prior to having the digital system — whether they’re fabricated in-house or sent out to the lab, taking into account the payments on the system that we’re utilizing, lab bill, cost of burs, blocks, data plan, all of the bells and whistles — I’ve found a significant return on investment in our office. Prior to utilizing the system, we were spending about $2,000 more per month than we’re spending now. So, yes, we have seen a return on investment.
With that being said, there’s also a bigger factor when you look at return on investment, and that’s personal satisfaction. I can tell you that with the quality of dentistry that you’re going to be able to provide after going digital — as well as the time that you’re going to save and the efficiency that it’s going to create in your office — you’ll have a level of personal satisfaction that is better than any monetary ROI that you could receive. You’re going to be very personally satisfied. And your patients will be happier because they’ll receive their crown faster whether you’re sending the case to the lab or milling it in-office for a same-appointment restoration. But you’d have to run the numbers for your individual practice and see if it works out for you. You can definitely make this a financially sensible — and more profitable — alternative to conventional impressions.
Is digital technology at a strong enough entry point, or do you still foresee major improvements? In other words, should I join in digital now or should I wait?
CD: One consideration is that about 20 percent of dentists across the United States have gone digital. When you look at the old marketing paradigm, that’s called “crossing the chasm” — what it takes for people to move on and adopt technology. And it’s usually at about 15 or 16 percent that we start seeing rapid movement. At 20 percent, we’re starting to see rapid movement. And that’s attributed to the accuracy of the systems and the success that both the doctors and the laboratories are seeing with it.
Now is the time to go digital. But before you make the leap, you should talk to your colleagues and your laboratory and find out what systems they’re recommending and what system will work best in your office.
What have you been doing differently since going digital that has significantly changed your practice?
CD: Before I went digital, I thought digital was just going to be for crown & bridge. But what I’ve realized is that there are so many capabilities of the system. We’re making partials, nightguards and clear aligners. We’re using it for advanced implant planning with our surgeons and laboratory. And we’re also using it for digital smile design, which I really wasn’t doing with traditional impressions. I really wasn’t doing clear aligners either, but now I’m starting to get more and more into that because the digital workflows are so convenient and so efficient, and we’re finding great success with them.

Dr. Chad Duplantis discussed the benefits of digital technology and the versatility of in-office milling.
ANAMARIA MURESAN, DMD, ME, CDT

In her presentation “New Techniques for Successful Veneers,” Dr. Anamaria Muresan described straightforward, predictable techniques for providing esthetic veneers.
How do you break contacts after cementing multiple veneers at the same time?
Dr. Anamaria Muresan: I like to use the serrated strips from ContacEZ® (ContacEZ; Vancouver, Wash.). At about 0.3 mm thick, they are very thin and delicate. For more tenacious situations, I like to use the Jiffy® Proximal Saw (Ultradent Products, Inc.; South Jordan, Utah), which comes in a 0.4 mm size. I also use a microbrush to wipe off the excess before curing.

Sharing techniques for esthetic veneers, Dr. Anamaria Muresan presented to a packed auditorium.

Dr. Muresan carefully relieves veneer contacts using the ContactEZ serrated strip.
PARESH PATEL, DDS
In his presentation “Monolithic Zirconia from Single Crowns to the Full Arch,” Dr. Paresh Patel explored the capabilities of monolithic zirconia, as well as the art and science of the material.
What is the minimum vertical restorative space for a full zirconia implant bridge?
Dr. Paresh Patel: The beauty of the solid zirconia bridge, and particularly the BruxZir® Full-Arch Implant Prosthesis, is that because it’s monolithic, we’re not stacking any kind of porcelain over the top of that; we’re not adding pink, layered porcelain or feldspathic porcelain for the gingival shade. We can significantly reduce the vertical requirements. With a minimum of 10 mm vertical clearance, you can prescribe a full-arch BruxZir implant restoration for your patient and avoid having to do aggressive bone reduction in the maxillary arch. Of course, you may have to remove some maxillary bone so that the transition line from prosthesis to mucosa is hidden under the lip line, but if you have 10 mm, then you’re going to have the bulk strength that you need of the monolithic zirconia to provide your patient with a durable, long-lasting BruxZir Full-Arch Implant Prosthesis.

Dr. Paresh Patel covered the art and science of monolithic zirconia, and the benefits this material affords patients.
JUSTIN CHI, DDS, CDT

In his presentation “The Reengineered PFM,” Dr. Justin Chi described one of the most frequently used restorations in dentistry — the PFM — and how it’s been reengineered using Obsidian® lithium silicate (Glidewell Laboratories; Newport Beach, Calif.), a remarkable new material.
What is the strength of Obsidian Fused to Metal compared to BruxZir Solid Zirconia?
Dr. Justin Chi: Obsidian Fused to Metal was created to address the primary flaw of porcelain fused to metal restorations: the weakness of feldspathic porcelain. The strength of Obsidian Fused to Metal is 397 MPa, which is four times stronger than conventional feldspathic porcelains and two times more chip-resistant. BruxZir Solid Zirconia is monolithic and available in multiple formulations, including: BruxZir Esthetic, which exhibits an average flexural strength of 870 MPa; and BruxZir Full-Strength, which exhibits an average flexural strength of 1,150 MPa.
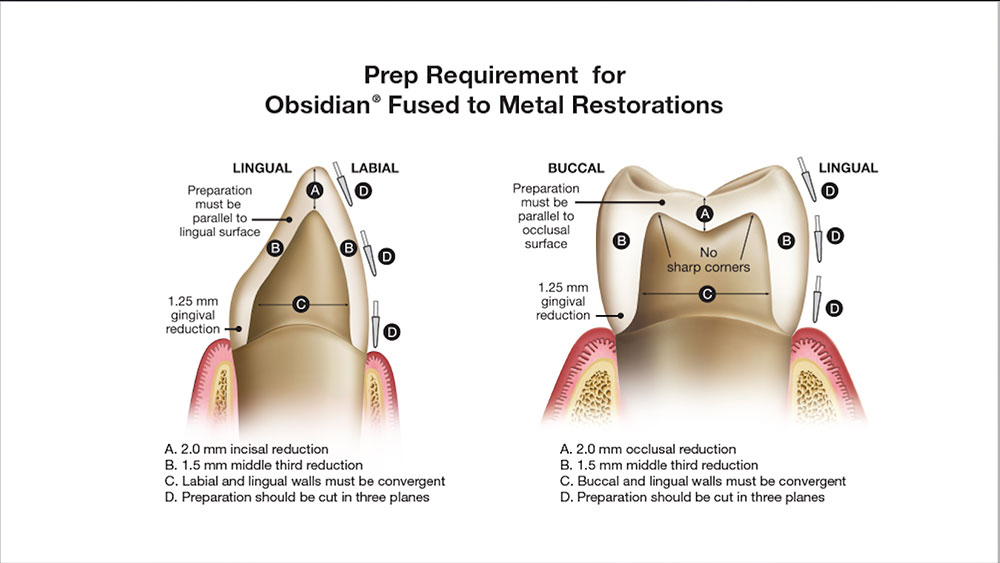
What are the prep requirements for Obsidian Fused to Metal crowns?
JC: With Obsidian Fused to Metal, for anterior crowns and bridges, you need 2.0 mm of incisal reduction and 1.5 mm of facial reduction utilizing a shoulder or chamfer margin. For posterior crowns and bridges, you should prep 2.0 mm from the occlusal, measuring from the deepest occlusal pit. Reduce the proximal by 1.5 mm and create either a 360-degree shoulder or deep chamfer margin.

Dr. Justin Chi outlined the unmatched strength and esthetics now achievable with Obsidian Fused to Metal restorations.
After tooth preparation, how long do you have the patient wear the provisional prior to taking the final impression?
Dr. Steven Barrett: Here are my considerations: 1) If I’ve done a gingivectomy or some minor gingival recontouring, then I typically wait about 21 days before I take the final impression. 2) In other cases, if a periodontist has done a crown-lengthening procedure, I typically wait six to eight weeks or until the periodontist tells me that I’m able to move forward with the case. 3) Sometimes there’s just regular gingival inflammation due to poor hygiene, and in those cases I may keep the provisional in place for two to three weeks and have the patient on a chlorhexidine rinse regimen.
What materials do you use to add length or close contacts on the provisionals?
SB: With BioTemps® Provisionals (Glidewell Laboratories), I simply use composite. I lightly roughen the surface, place a little bonding agent, and then add the composite and contour it. It polishes and blends beautifully with our provisionals.
If the provisionals are too nice, will the patient come back for the rest of the treatment?
SB: I guess my question to you is, “If your temporaries are not that nice, are you concerned that the patients won’t come back?” In dental school we were taught that if your temporaries were too nice, the patients won’t show up. However, my temporaries are actually a referral source for me. You have to imagine that your patients have to go to work, and they have to be with their friends and family. If they have anterior provisionals in place, you want them to be as esthetic and natural as possible.
During my symposium presentation, I talked about thinking about your provisionals as your business card. This is what everyone else is going to see, and you want your patients to speak highly of you and your staff. If they have provisionals that are not contoured properly, or the color or shade is off, they’re not going to be a great referral source for you. Just keep that in mind. Spend the time to teach yourself how to do it and also to train your staff.
Do you contour all of the provisionals yourself?
SB: No. I do a lot of them myself, especially when I’m traveling to offices, working with staff, and teaching doctors and staff. But when I’m in my own office working, my staff, who’s been with me for over 10 years, will contour them about 80 percent of the way. And then my job is to go in and use my artistic ability and customize the provisional for the patient. Whether it’s the contour, the incisal edge length or those incisal embrasures, I’m personalizing them for each patient.
Teach your staff how to get you 80 percent of the way, and then the other 20 percent you’re going to have to do yourself, possibly. That’s a nice time for you to interact with patients, and it’s an opportunity for them to experience you as a dentist and the caring nature that you have as you customize their provisionals. They’re really going to appreciate that. Most of the time they’re going to tell you that they’ve never been to a dentist that’s taken that much time to really make sure that these are perfect. Now you have a great stepping stone that the lab can use for the final case. So whether you document it in a photograph or a study model, you have a way to communicate to the lab how to get your final restorations exactly the way that you and the patient would like them.

Dr. Steven Barrett described how esthetic provisionals can be viewed as a business card — to reflect the high-quality work of the practice.



